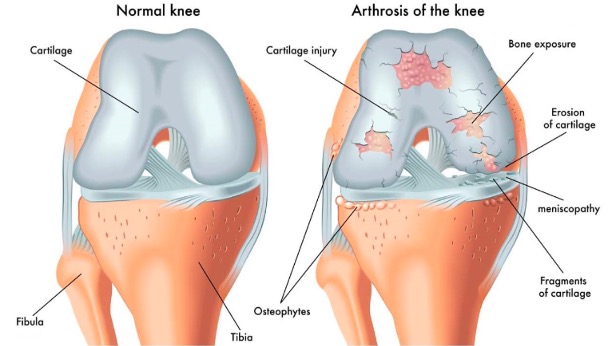
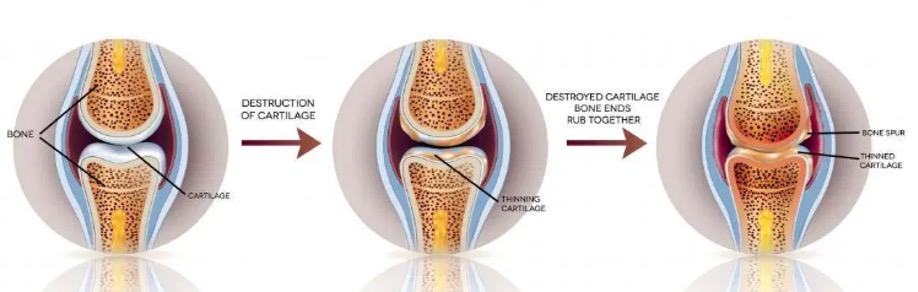
Osteoarthritis (OA) is a joint disease that is characterised by damage to the joints which affects synovial fluid, cartilage, bones, muscles, blood supply and nerves. It happens when the protective cartilage that covers the tips of our bones is gradually worn down and this causes multiple bones to rub against each other. This ultimately leads to pain and eventual loss of function.
Osteoarthritis also affects other connective tissues and muscles related to the affected joint. For example, knee osteoarthritis may affect the connective tissues and muscles in the thighs, calf, buttock and even other joints like the hip and ankle. Having said that, OA does not only affect the knee joint, it also affects the joints in the hands, hips, and spine.
Proper use of the joints will keep it lubricated and this stimulates the repair and rebuilding process. On the other hand, lack of joint use causes the cartilage to become dryer, more brittle and more prone to damage over time. This tends to happen in the parts of the joint surface that is related to ranges of motion that are not being used sufficiently. As time passes, the damage and pain become so severe that it leads to deformities that cannot be corrected and this would leave surgery as the only option.
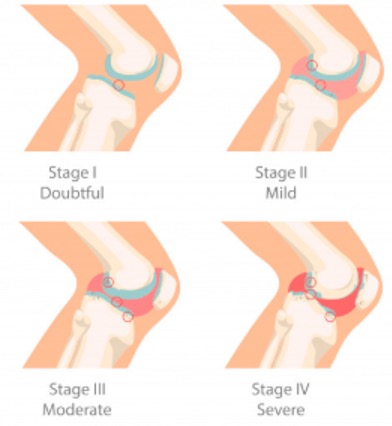
The 5 Stages of Knee OA
OA of the knee progresses in stages and takes many years to develop. This condition can be hard to treat because symptoms may not appear until OA reaches an advanced stage. OA is divided into five stages (5) with stage 0 representing a healthy & stable knee. As the stages progress, pain and stiffness increase. Here we will focus on the 4 Stages of OA, from Minor to Severe.
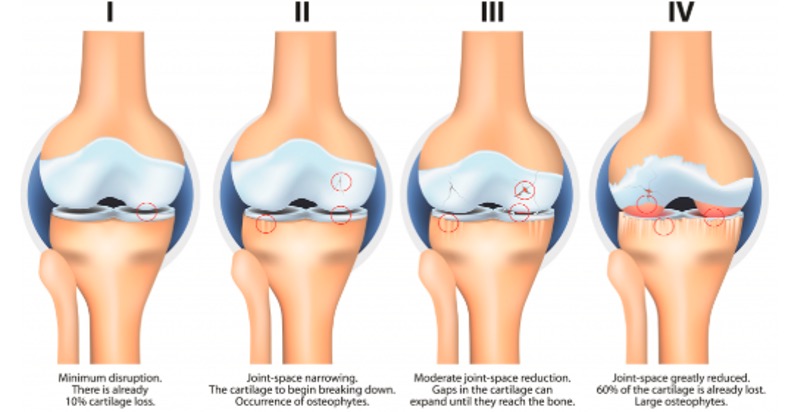
Stage 1 - Minor / Doubtful
- Minor wear and tear of the cartilage
- Minor bone spurs
- Unlikely pain or discomfort due to minor wear and tear only
Stage 2 - Mild
- Greater bone spurs
- Synovial fluid starts to decrease
- Cartilage still intact
- Start to feel pain after prolonged walking, and more stiffness when the joint is not being used with mild tenderness when kneeling
Stage 3 - Moderate
- Cartilage damage and joint space starts to narrow
- Joint stiffness after prolonged inactivity
- Joint swelling
- Frequent pain while walking
Stage 4 - Severe
- Cartilage almost completely gone and joint space is extremely narrow
- Severe pain and discomfort during rest and simple activities like walking
Primary Osteoarthritis vs Secondary Osteoarthritis
Osteoarthritis can be classified into 2 categories:
- Primary (or idiopathic): Most common type of OA, the exact cause being unknown (in the large majority of cases) but it is not a result from any injury or disease, rather it is said to be associated to certain risk factors, such as, age, sex, obesity, genetic, job hassle and etc.
- Secondary: Occurs with another disease or condition, such as an infection, a joint abnormality that appeared at birth, an injury, or metabolic disorders that cause excessive iron in the body or excess copper in the liver.
Who Tends to get OA?
Symptomatic knee OA is currently the fourth leading cause of disability worldwide, [4] with an estimated prevalence of 70–80% in the population aged 55 years and older [5]. An ageing Asia with longer lifespan suggests ever-greater numbers of knee OA, among other chronic conditions [6]. The point prevalence of knee OA in Malaysia today is estimated to be 10–20% of the total adult population [7].
- Older people. Cartilage deteriorates naturally with age. It is affecting more than half of the population that is over the age of 65. Although it is more prominent in the later stages of life, some younger people may be affected by it too. According to The Star (6th August 2019), one in three Malaysians over the age of 55 suffers osteoarthritic pain.
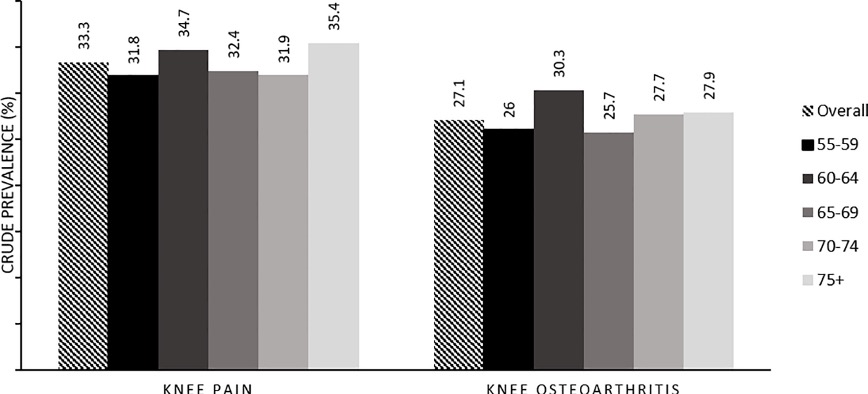
Source: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0225075
- Gender. Women are more likely to develop osteoarthritis, though it is not clear why. It is believed that the hormone oestrogen protects the cartilage from inflammation and women tend to lose that protection after menopause when oestrogen level drops. Besides that, wider hips in women compared to men may cause extra stress on the insides of the knee, making women have a higher risk of getting OA when compared to men.
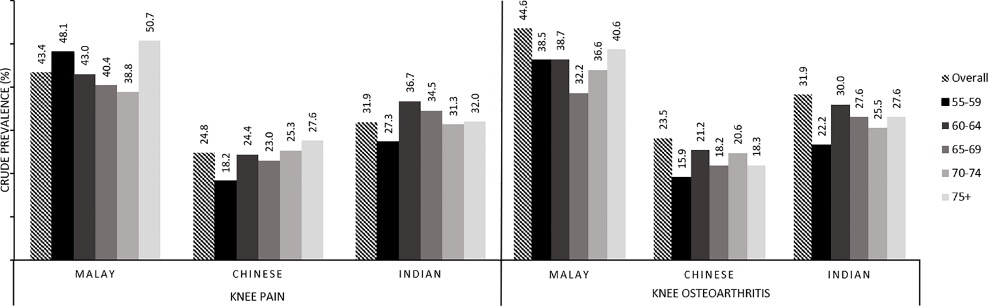
Source: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0225075
- Obesity. Based on 2019 WHO global estimates of obesity and overweight data, Malaysia has the highest rate in Asian countries; therefore, weight related joint disease such as OA is indeed one of the main knee problems in Malaysia. Also, fat tissue produces proteins that can cause harmful inflammation in and around the joints which increase the chances of getting OA.
- Joint injuries. Weak joints are more susceptible to OA. OA may develop as a secondary consequence of joint damage from rheumatoid arthritis, gout or other arthritic conditions.
- Repeated stress on the joint. Physically demanding jobs or a sport that places repetitive stress on a joint can increase the chance of developing OA.
- Genetics. The only clear genetic link is called nodal osteoarthritis, which affects the small hand joints in older women and runs in families.
- Bone deformities. Some people are born with malformed joints or defective cartilage such as knock knee and bow knee which may lead to OA in the later stages of life.
- Certain metabolic diseases. Diseases like diabetes may slow down the healing process within the joint.
- Surgery or Trauma. Repair of the cartilage, ligaments and menisci (the small spacers in the knee) can restore normal function to a joint, but around 50-60% of patients develop osteoarthritis to some degree from five to fifteen years later.
- Chronic lower back pain. People tends to adjust themselves to a more comfortable position to avoid the pain and this causes muscle imbalance in our lower extremities which may develop into OA as time passes.
Which Joints Get Osteoarthritis?
While osteoarthritis can occur in any joint due to injury or abnormality it is much more common in certain joints, particularly weight bearing ones. It is often symmetrical, occurring to some degree in joints on both sides.

- Knees. Common in older people, especially women. If severe may lead to total knee replacement.
- Hips. Again common in older people and may require total hip replacement.
- Spinal. The small joints in the back and neck (not the major disc joints) can become arthritic and give stiffness, pain and limited movement.
- Hands. The small hand joints may develop bony swelling, become stiff and go off at angles to straight. The most common and troublesome is the joint at the base of the thumb.
- Big Toe. This joint is susceptible to changes in the same way as the base of the thumb.
We shall look into the signs and symptoms of OA and how Oxidative Stress can lead to OA in our next Blog.
Learn more how Hi-Bliss Hydrogen Therapy can help slow down the progression of OA here : https://hi-bliss.com/muscle-joint-programs/
References:
- “The epidemiology of osteoarthritis in Asia,” International Journal of Rheumatic Diseases, vol. 14, no. 2, pp. 113–121, 2011.
- “Pain in osteoarthritis,” African Journal Biomedical Research, vol. 11, no. 2, pp. 119–128, 2008
- “Tibiofemoral osteoarthritis affects quality of life and function in elderly Koreans, with women more adversely affected than men,” BMC Musculoskeletal Disorders, vol. 11, article 129, 2010.
- Clinical Practice Guidelines on the Management of Osteoarthritis, Ministry of Health Malaysia, 2010
- https://springloadedtechnology.com/guide-to-severe-knee-osteoarthritis/
- https://www.mayoclinic.org/diseases-conditions/osteoarthritis/symptoms-causes/syc-20351925
- https://www.healthline.com/health/osteoarthritis#osteoarthritis-symptoms
- https://www.arthritis.org/diseases/osteoarthritis
- https://www.webmd.com/osteoarthritis/default.htm