If you are experiencing signs your body has inflammation, it can crop up in the form of various symptoms and be a sign of a number of different health concerns. Usually, inflammation is associated with joint health since arthritis is one of the top causes of pain and swelling. But inflammation can be associated with other health concerns, beyond swollen joints.
Keep in mind that not all inflammation is bad. Acute inflammation is important to our health because it helps us heal. Think about when you twist your ankle and it becomes hot, red, and swollen. That is part of your body's response to help heal the injury." And it will go away, once your ankle is healed.
What you want to watch out for are signs of chronic inflammation - This is the type of inflammation that does more harm than good. "Think of chronic inflammation like a fire that needs to be put out in the body. Chronic inflammation has a domino effect where it can trigger a cascade of symptoms that can negatively impact your health."
Here are a few signs you have too much inflammation, according to experts:-
Let’s look at the Foods That Reduce Inflammation in the next blog.
Learn more how Hi-Bliss Hydrogen Therapy can help reduce Inflammation here : https://wordpress-851564-2937612.cloudwaysapps.com/what-is-hibliss-hydrogen-therapy/
Sources:
Based on visual observation, the ancients characterised inflammation by five cardinal signs, namely redness (rubor), swelling (tumour), heat (calor; only applicable to the body' extremities), pain (dolor) and loss of function (functio laesa).
More recently, inflammation was described as "the succession of changes which occurs in a living tissue when it is injured provided that the injury is not of such a degree as to at once destroy its structure and vitality", or "the reaction to injury of the living microcirculation and related tissues”.
The classical description of inflammation accounts for the visual changes seen. Thus, the sensation of heat is caused by the increased movement of blood through dilated vessels into the environmentally cooled extremities, also resulting on the increased redness (due to the additional number of erythrocytes passing through the area). The swelling (oedema) is the result of increased passage of fluid from dilated and permeable blood vessels into the surrounding tissues, infiltration of cells into the damaged area, and in prolonged inflammatory responses deposition of connective tissue.
Pain is due to the direct effects of mediators, either from initial damage or that resulting from the inflammatory response itself, and the stretching of sensory nerves due to oedema. The loss of function refers to either simple loss of mobility in a joint, due to the oedema and pain, or to the replacement of functional cells with scar tissue.
Today it is recognised that inflammation is far more complex than might first appear from the simple description given above and is a major response of the immune system to tissue damage and infection, although not all infection gives rise to inflammation. Inflammation is also diverse, ranging from the acute inflammation associated with S. aureus infection of the skin (the humble boil), through to chronic inflammatory processes resulting in remodeling of the artery wall in atherosclerosis; the bronchial wall in asthma and chronic bronchitis, and the debilitating destruction of the joints associated with rheumatoid arthritis .
In short, Inflammation is a vital part of the immune system's response to injury and infection. It is the body's way of signaling the immune system to heal and repair damaged tissue, as well as defend itself against foreign invaders, such as viruses and bacteria. Inflammation is considered the cornerstone of pathology in that the changes observed are indicative of injury and disease.
Without inflammation as a physiological response, wounds would fester, and infections could become deadly. However, if the inflammatory process goes on for too long or if the inflammatory response occurs in places where it is not needed, it can become problematic. Chronic inflammation has been linked to certain diseases such as heart disease or stroke, and may also lead to autoimmune disorders, such as rheumatoid arthritis and lupus.
There are 2 types of inflammation – the “Good” or protective type (which benefits health) and the “Bad” or harmful type (which destroys it).
Inflammation happens when a physical factor triggers an immune reaction. Inflammation does not necessarily mean that there is an infection, but an infection can cause inflammation.
Acute inflammation can result from:
When the body detects damage or pathogens, the immune system triggers a number of reactions:
Signs of acute inflammation can appear within hours or days, depending on the cause. In some cases, they can rapidly become severe. How they develop and how long they last will depend on the cause, which part of the body they affect, and individual factors.
Some factors and infections that can lead to acute inflammation include:
Chronic inflammation can develop if a person has:
Factors that may increase the risk of chronic inflammation include:
Chronic inflammation can continue for months or years. It either has or may have links to various diseases, such as:
Diabetes | Cardiovascular disease (CVD) | Arthritis and other joint diseases | Allergies | Chronic obstructive pulmonary disease (COPD) | Psoriasis | Rheumatoid Arthritis
The symptoms will depend on the disease, but they may include pain and fatigue.

For example, chronic inflammation has been linked to heart disease and stroke. One theory suggests that when inflammatory cells stay too long in blood vessels, they promote the buildup of plaque. The body perceives this plaque as a foreign substance that doesn't belong, so it tries to wall off the plaque from the blood flowing inside the arteries, according to the American Heart Association (AHA). If the plaque becomes unstable and ruptures, it forms a clot that blocks blood flow to the heart or brain, triggering a heart attack or stroke.
Cancer is another disease linked with chronic inflammation. Over time, chronic inflammation can cause DNA damage and lead to some forms of cancer, according to the National Cancer Institute.
Chronic, low-grade inflammation often does not have symptoms, but doctors can test for C-reactive protein (CRP), a marker for inflammation in the blood. High levels of CRP have been linked with an increased risk of heart disease. CRP levels can also indicate an infection, or a chronic inflammatory disease, such as rheumatoid arthritis or lupus, according to the Mayo Clinic.
Besides looking for clues in the blood, a person's diet, lifestyle habits and environmental exposures can contribute to chronic inflammation. It is important to maintain a healthy lifestyle to keep inflammation in check.
The following table summarizes some key differences between acute and chronic inflammation:

Let’s look at Signs of you have Inflammation and more on Chronic Inflammation – The New Silent Killer in more depth in the next blog.
Learn more how Hi-Bliss Hydrogen Therapy can help reduce Inflammation here : https://wordpress-851564-2937612.cloudwaysapps.com/what-is-hibliss-hydrogen-therapy/
Sources:
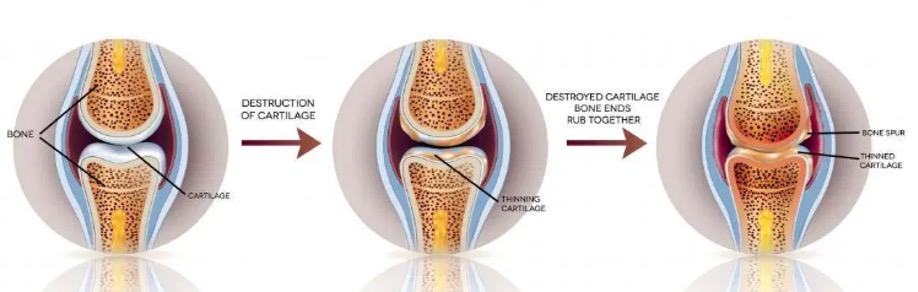
Osteoarthritis (OA) is a joint disease that is characterised by damage to the joints which affects synovial fluid, cartilage, bones, muscles, blood supply and nerves. It happens when the protective cartilage that covers the tips of our bones is gradually worn down and this causes multiple bones to rub against each other. This ultimately leads to pain and eventual loss of function.
Osteoarthritis also affects other connective tissues and muscles related to the affected joint. For example, knee osteoarthritis may affect the connective tissues and muscles in the thighs, calf, buttock and even other joints like the hip and ankle. Having said that, OA does not only affect the knee joint, it also affects the joints in the hands, hips, and spine.
Proper use of the joints will keep it lubricated and this stimulates the repair and rebuilding process. On the other hand, lack of joint use causes the cartilage to become dryer, more brittle and more prone to damage over time. This tends to happen in the parts of the joint surface that is related to ranges of motion that are not being used sufficiently. As time passes, the damage and pain become so severe that it leads to deformities that cannot be corrected and this would leave surgery as the only option.
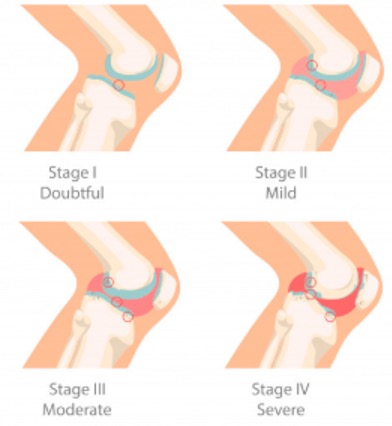
OA of the knee progresses in stages and takes many years to develop. This condition can be hard to treat because symptoms may not appear until OA reaches an advanced stage. OA is divided into five stages (5) with stage 0 representing a healthy & stable knee. As the stages progress, pain and stiffness increase. Here we will focus on the 4 Stages of OA, from Minor to Severe.
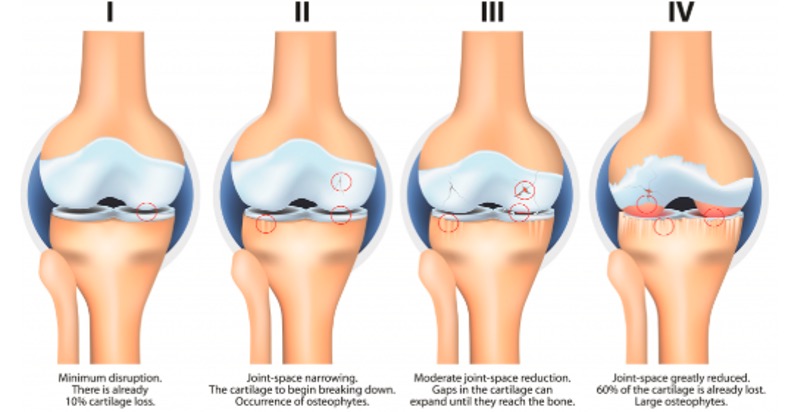
Stage 1 - Minor / Doubtful
Stage 2 - Mild
Stage 3 - Moderate
Stage 4 - Severe
Osteoarthritis can be classified into 2 categories:
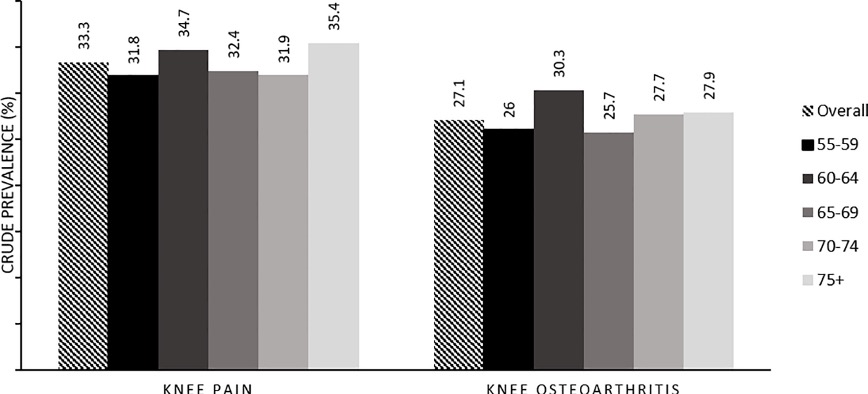
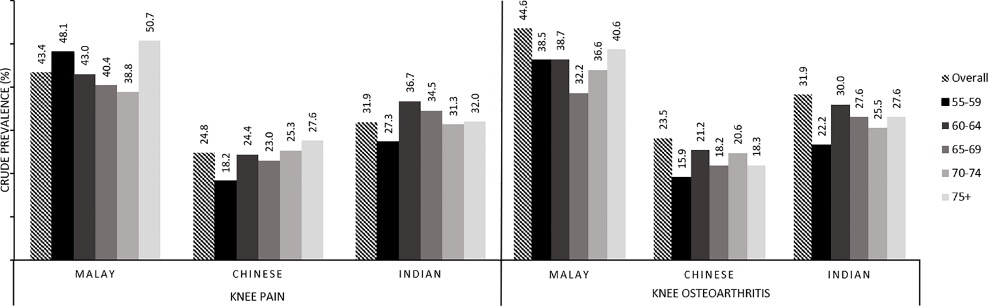
Symptomatic knee OA is currently the fourth leading cause of disability worldwide, [4] with an estimated prevalence of 70–80% in the population aged 55 years and older [5]. An ageing Asia with longer lifespan suggests ever-greater numbers of knee OA, among other chronic conditions [6]. The point prevalence of knee OA in Malaysia today is estimated to be 10–20% of the total adult population [7].
While osteoarthritis can occur in any joint due to injury or abnormality it is much more common in certain joints, particularly weight bearing ones. It is often symmetrical, occurring to some degree in joints on both sides.

We shall look into the signs and symptoms of OA and how Oxidative Stress can lead to OA in our next Blog.
Learn more how Hi-Bliss Hydrogen Therapy can help slow down the progression of OA here : https://hi-bliss.com/muscle-joint-programs/
Atopic dermatitis (also known as AD), is the most common type of eczema, a skin condition that makes you itch and leaves red blotches, usually on your face, arms, and legs. Atopic dermatitis is a common and often persistent skin disease that affects a large percentage of the world's population. The rashes tend to flare and go away, but then come back again.
Atopic dermatitis typically begins in childhood, usually in the first six months of a baby’s life. Even though it is a common form of eczema, it may become severe and lifelong nuisance. Normally, AD disappears as a child grows older, but some adults could still suffer from AD flare ups.
“Atopic” refers to an allergy. Atopic dermatitis also usually exists alongside two other allergic conditions, which are asthma and hay fever (allergic rhinitis). People who have asthma, hay fever or have family members with AD are more likely to develop it.
Types of Atopic Dermatitis
Signs & Symptoms of Atopic Dermatitis (eczema) include:


There is no exact reason behind atopic dermatitis but research shows a combination of genetics and external factors that may be involved. A study published by Nature Genetics found that some people with eczema lack the proper proteins to build a strong barrier on the outer most layer of the skin (epidermis).
This group of people, especially those with atopic dermatitis may have partial or complete mutation on the gene responsible for creating a protein known as filaggrin. Filaggrin helps our bodies maintain a healthy, protective barrier on the epidermis.

This genetic mutation causes a lack of filaggrin in the epidermis layer which leads to a reduction in the ability to maintain the skin’s natural amount of water and thus results in dry skin which causes itchiness. Lack of filaggrin may also allow allergens to enter the skin which will then trigger an inflammatory response by the immune system, causing inflammation that again results in red, rash and itchy skin. This is the main reason why many people who suffer from atopic dermatitis tend to have extremely dry and infection-prone skin.


Atopic dermatitis (AD), affecting 2 to 3-fold in industrialized nations, impacting approximately 20% of children and 3% of adults worldwide.
Those who live in developed countries or colder climates seem to be more likely to develop AD.
Studies have found that 33% to 67% of children and young people with AD also have some food allergies. Moreover, general aspects of AD will affect between 8% to 18% of infants and young children.
Around 50% of people who suffer from atopic dermatitis develop symptoms within their first year of life, and probably as many as 95% experience an onset of AD when they are below five years of age. Around 75% of people with the childhood onset of the disease have seen their symptoms decrease before adolescence. The remaining 25% continue to have eczema during adulthood or may experience a relapse of symptoms after some years without experiencing any symptoms.

Around 50–75% of all children with early-onset atopic dermatitis are sensitive to allergens.
Examples of allergens include pets, house dust mites or even food allergens, whereas those with late-onset atopic dermatitis are often less sensitive to these allergens.
Atopic dermatitis is more than just a skin condition known as the “itch that rashes”. It is a disease caused by an overactive immune system that leads to inflammation in the body. It is also the main culprit behind internal inflammation that causes the symptoms to flare up. Besides that, scratching may lead to only temporary relief and may worsen the itching in the long run. This is called the itch-scratch cycle.

In healthy skin, the outer layer (epidermis) keeps foreign substances such as bacteria, viruses and allergens from entering the body. When you have atopic dermatitis, the outer layer of the skin is weaker and is more vulnerable to inflammation as a result of immune cells in the body. The damage done by scratching also contributes to the breakdown of skin cells which makes it easier for foreign substances to enter the body.
Once these foreign substances have broken through the skin barrier, immune cells alert the body that it is under attack. These immune cells travel to the lymph nodes at the dermis called as the second layer of the skin. Once they have entered the lymph nodes, these immune cells activate your body’s protectors, called T helper cells.
The immune cells release substances which cause redness and rashes on the skin. This will cause the inflammatory process to continue, so the skin reacts even when it looks clear. Even when the rash cannot be seen clearly, the underlying inflammation is still active beneath the skin. People tend to scratch when they feel itchy, and this further weakens the skin cells in the epidermis which allow more foreign substances to get in and this ultimately would increase the risk of infection.
Studies have shown that almost 50% - 70% of children and 7% - 9% of adults with severe atopic dermatitis will develop asthma.

Doctors and scientist came up with theories as to why a skin rash is associated with asthma. Does immune system disorders cause an overreaction to allergens that are in contact with the skin and lung airways or is it the defective skin and airways that trigger an excessive immune response?
A research by Dr. Kopan suggested that the problems started with the damaged or defective skin itself. The researchers found that cells in the damaged skin can secrete thymic stromal lymphopoietin (TSLP), a compound that is able to cause an immune response and due to the skin’s effectiveness in secreting TSLP into the blood system, the substance travels throughout our body, causing AD flares up. When it reaches our lungs, it then triggers the hypersensitive characteristics of respiratory problems which could lead to asthma attacks.
Let us learn more about what causes atopic dermatitis or flare-ups/ triggers, our Skin and more on how to reduce the effects of Atopic Dermatitis in our next Blog.
Learn more how Hi-Bliss Hydrogen Therapy can help you manage your Skin Condition here : https://hi-bliss.com/skin-eyecare-programs/

Your skin might be fine for a long time. But then something happens to cause a rash or itchiness. Some things that trigger atopic dermatitis or make it worse include:
Natural remedies to ease your Atopic Dermatitis Flare-Ups/ Triggers
Though there is no known cure for Atopic Dermatitis, Eczema, these are a few natural remedies to help you ease and manage your AD flare-ups.
Hydrogen is the first component of the periodic table. The most important function of hydrogen in the human body is to keep you hydrated. Water is made up of hydrogen and oxygen and is absorbed by the cells of the body.
Hydrogen contains dissolved molecular hydrogen, which can ease oxidative stress and has shown therapeutic effects in several pathological conditions, including AD. It is an element which is present in all the fluids of the human body which allows the toxins and waste to be transported and eliminated properly. Hydrogen has also been reported to increase glutathione peroxidase activity, downregulate thymus and activation-regulated chemokine (TARC).
These are implicated in the pathogenesis of AD and used as an indicator of disease severity. Thymus and activation-regulated chemokine binds to the chemokine receptor CCR4 and induces chemotaxis in T cells, therefore acting as a proinflammatory factor in AD. It has been suggested that H2 may have therapeutic potential in AD by reducing TARC.


In conclusion, hydrogen is a safe and effective medical gas that has been proven to be able to treat and control various diseases. It can suppress the levels of inflammation related mediators such as Th1, Th2, and pro-inflammatory cytokines which are the main cause in the development of diseases such as atopic dermatitis in the human body. In conclusion, Hydrogen has cemented its place as an alternative preventive treatment for AD that is also beneficial to the human body.
The SKIN is the largest and fastest-growing organ in the body. It has several important functions such as:
The skin is made up of several layers, which protect the body from pressure, temperature, micro-organisms, radiation and chemicals.

The liver is the only organ in our body that can repair itself. It has a variety of functions like the ability to break down toxins, deactivate hormones, filter waste products to the bowels & kidneys, and to store nutrients such as vitamins A, D and B12. Due to this, the digestive and elimination systems which include the skin and kidneys may be affected by a sluggish liver.
When the liver is exhausted, it is unable to eliminate toxins. Other organs such as the kidneys and skin are forced to replace its role to eliminate toxins and wastes out from the body via the epidermis. This can disrupt the skin, especially if it is already sensitive or is inflicted with eczema. These toxins can easily cause irritation, itchiness and even a dreaded flare-up.


OA is diagnosed by a triad of typical symptoms, physical findings, and radiographic changes. The American College of Rheumatology has set forth classification criteria to aid in the identification of patients with symptomatic OA that include, but do not rely solely on, radiographic findings. Diagnosis of Osteoarthritis is done by noting the signs and symptoms:

There are several ways in which OA can impact the quality of life such as increasing stress and sleep disruption due to pain that has intensified. Osteoarthritis also reduces the ability to perform normal activities in our daily life and reduces productivity. It can also lead to problems with anxiety and depression.
Pain and stiffness can decrease your desire to be active. Not only does a lack of activity limit your enjoyment of life — it can also reduce muscle mass which leads to muscle tightness and a risk of falling and suffering from other injuries. Muscles are more prone to injury when it is tight or weak, and micro-tears lead to scarring of the muscles that can disrupt normal muscle function, therefore affecting the surrounding connective tissues.
Lack of activity can also lead to weight gain. Extra weight may exacerbate OA symptoms, and this may lead to an increased risk of getting other complications such as:
Other complications that can arise from OA are:

A number of factors may put a person at risk of developing OA. Making changes may not prevent the condition, but a person may be able to reduce their risk or keep OA from advancing.
The Arthritis Foundation suggest the following:




Oxidative stress happens when there is an imbalance between the number of free radicals and antioxidants in our body. This is particularly harmful as it can lead to cell and tissue damage. Oxidative stress is considered a main causative factor in the pathogenesis of OA. Many pro-inflammatory mediators or free radicals are elevated in OA, including Reactive Oxygen Species (ROS), and Reactive Nitrogen Species (RNS).

The excessive production of free radicals can harm cell functionality as it damages cellular lipids, proteins and DNA. Free radicals can give rise to cartilage apoptosis/ cell death, thus accelerating articular cartilage dysfunction and degeneration.

Oxidative stress is known to be detrimental to many cells and to occur during disease and with ageing. It has also been implicated in the development of OA. Although osteoarthritis has been traditionally classified as a non-inflammatory arthritis, however evidence has increasingly shown that inflammation occurs as cytokines and metalloproteinases are released into the joint. Inflammation get worse when more of these agents are released, especially when triggered by excessive free radicals. Inflammation in the cartilage and synovial leads to loss of joint structure and progressive damage to the cartilage, causing OA to become worse. Inflamed articular cartilage still remains a huge hurdle to treat due to the limited self-healing capacity of the cartilage which lacks nerves and blood supply.
Hydrogen therapy is one of the newest and most effective treatments to manage arthritis due to its role as a therapeutic antioxidant. It is able to selectively neutralize free radicals in the affected area which reduces inflammation and prevents further damage to the joint, thereby slowing down the progression of OA. As hydrogen is the smallest molecule on earth, it is able to diffuse itself into the targeted cells without affecting the functions of other cells and organs.
Based on a research by Ding Li and Wan Chun Wang in the year of 2012, hydrogen is considered to be a selective antioxidant and can be used as a kind of therapeutic medical gas. This further reinforces the idea that hydrogen treatment can help to decrease the damage of cartilage caused by oxidative stress.
In Hi-Bliss Hydrogen therapy centre, we combine the therapeutic benefits of hydrogen therapy with osteopathic manual practices. Our certified physiotherapist will perform the Osteopathic Structural and Functional Examination on the lower limb area to find out the root cause of the pain by measuring the Range of Motion (ROM), Muscle Strength, Gait Analysis, Posture Alignment, Quality of Movement, Pain during Movement, Muscle Bulk and Tone. The hydrogen treatment aims to suppress inflammatory factors such as free radicals and slow down the progression of osteoarthritis.
By combining the Hydrogen with Osteopathic practices, we help our clients reduce pain in the joint, slow down the progression of OA and ultimately help them return to normal daily life. Hydrogen therapy is efficient in treating the inflamed joints caused by OA by repairing the internal cells in our body while our physiotherapy/osteopathic techniques helps to improve the external muscles caused by muscle imbalance. We will also educate clients about suitable stretching and strengthening exercise that aims to manage symptoms and improve joint function, flexibility and balance.
By reducing the number of OA symptoms, it will improve your ability to get around and increase your quality of life.
Learn more how Hi-Bliss Hydrogen Therapy can help slow down the progression of OA here : https://wordpress-851564-2937612.cloudwaysapps.com/treatment-services-osteoarthritis-therapy/
How can you improve your immune system? Overall, your immune system does a remarkable job of defending you against disease-causing microorganisms. But sometimes it fails: A germ invades successfully and makes you sick. Is it possible to intervene in this process and boost your immune system? In order for our immune system (which is a complex system, not a single entity) to function well, it requires balance and harmony.
In this article we will share some helpful ways to strengthen your immune system and fight off diseases. A few lifestyle changes and new habits can naturally keep your immune system strong and healthy:

Eating a healthful, balanced diet can improve a person’s overall well-being.
For people with a weak immune system, doctors generally recommend a diet that is rich in vegetables and fruit, which will provide plenty of nutrients. 
If a person is very immunocompromised, for example, because they are undergoing cancer treatment, a doctor may recommend that they take extra steps to avoid foodborne illnesses.
These may include:

Stress has a significant effect on your immune system. During stress, a series of events release cortisol, adrenaline, and other stress hormones from the adrenal gland. Together they help your body cope with stress. Normally, cortisol is helpful because it decreases the inflammation in the body that results from the immune responses caused by stress.
But if a person is chronically stressed, stress hormones can affect the way the body functions over time. This increases your risk of health problems, including:

You do not need a reason to get a good night’s sleep, but now you have one – It Keeps you HEALTHY! According to the National Sleep Foundation, sleep deprivation has a similar effect on the body’s immune system as stress. Lack of sleep disrupts the normal production of white blood cells, a crucial component of the body’s immune system.
According to the CDC, adults should aim for at least 7 hours of sleep per day, while infants and children need between 8 and 17 hours of sleep depending on their age.
 Your body will be able to fight sickness a lot better if it is strong and healthy. Regular exercise keeps the body healthy. In addition to strengthening the body, exercise causes the body to release endorphins that reduce stress levels. However, those with weak immune systems should be careful not to push themselves too hard as this can weaken the immune system further.
Your body will be able to fight sickness a lot better if it is strong and healthy. Regular exercise keeps the body healthy. In addition to strengthening the body, exercise causes the body to release endorphins that reduce stress levels. However, those with weak immune systems should be careful not to push themselves too hard as this can weaken the immune system further.
Regular exercise is one of the pillars of healthy living. It improves cardiovascular health, lowers blood pressure, helps control body weight, and protects against a variety of diseases. It may contribute even more directly by promoting good circulation, which allows the cells and substances of the immune system to move through the body freely and do their job efficiently.
 Your body just functions better with water. Fill a big jug in the morning and drink it all. Alternatively, instead of just drinking normal water, consume at least 500ml or better still 1 liter of Hydrogen rich water daily for your overall health and wellness.
Your body just functions better with water. Fill a big jug in the morning and drink it all. Alternatively, instead of just drinking normal water, consume at least 500ml or better still 1 liter of Hydrogen rich water daily for your overall health and wellness.
Ref: https://www.oatext.com/pdf/JTS-6-380.pdf
Your liver does so much for you, so take care of it, especially during cold and flu months. 

Your immune system is the key to good health, so the more you can do to protect it, the better.
Let’s look at the foods that can help boost your Immune System in the next blog.
Because the immune system is so complex, there are many potential ways in which it can go wrong.
The types of immune disorders can fall into these three categories:
Immunodeficiencies
These arise when one or more parts of the immune system do not function. Immunodeficiencies can be caused in a number of ways, including age, obesity, and alcoholism. In developing countries, malnutrition is a common cause. AIDS is an example of an acquired immunodeficiency.
In some cases, immunodeficiencies can be inherited, for instance, in chronic granulomatous disease where phagocytes do not function properly.
Autoimmunity
In autoimmune conditions, the immune system mistakenly targets healthy cells, rather than foreign pathogens or faulty cells. In this scenario, they cannot distinguish self from non-self.
Autoimmune disorders are when the body mistakenly attacks healthy tissue, resulting in diseases. This is what occurs in people with autoimmune diseases such as:
Hypersensitivity
With hypersensitivity, the immune system overreacts in a way that damages healthy tissue. An example is anaphylactic shock where the body responds to an allergen so strongly that it can be life-threatening.

Anaphylaxis happens when the body reacts to a foreign substance as if it were a serious threat to health. The most common triggers for these reactions are medications, foods, and insect stings. In its reaction to an allergen, the body produces large amounts of histamine — a signaling molecule that can trigger an inflammatory response. This response can lead to:

In a person experiencing anaphylaxis, the airways often become narrow, making breathing difficult. In addition, the blood vessels may leak, causing edema, a type of swelling that results from the accumulation of fluid.
Signs of a weak Immune System
Most of the time, the immune system protects the body from infection. However, some people have a weak immune system that may make them prone to frequent infections. Here are some signs you might be having a weak Immune System:-
1. Susceptibility to infection.
A person with a weak immune system is likely to get infections more frequently than most other people. Infections that people with a weak immune system often get include: Pneumonia / Meningitis / Bronchitis / Skin Infections
2. You Always Have a Cold

It is perfectly normal for adults to sneeze and sniffle through two or three colds each year. Most people bounce back in seven to 10 days. During that time, it takes the immune system three to four days to develop antibodies and fight off pesky germs. But if you are constantly catching colds – or have a cold that would not run its course – that is a clear sign your immune system is struggling to keep up.
3. You feel constantly feel tired or fatigued

If you are getting enough sleep and still suffering from exhaustion, it is worth considering if your immune system is trying to tell you something. When your immune system struggles, so does your energy level. “That's because your body is trying to conserve energy to fuel your immune system so it can fight off germs,”
4. Your Stress Level is Sky-High
According to a report by the American Psychological Association, long-term stress weakens the responses of your immune system. “That’s because stress decreases the body’s lymphocytes, the white blood cells that help fight off infection. The lower your lymphocyte levels, the more you’re at risk for viruses like the common cold,” explains Nadia Hasan, DO, a physician at Delancey Internal Medicine.
5. Your Wounds Are Slow to Heal
Your skin goes into damage control mode after you get a burn, cut or scrape. Your body works to protect the wound by sending nutrient-rich blood to the injury to help regenerate new skin. This healing process depends on healthy immune cells. But if your immune system is sluggish, your skin cannot regenerate. Instead, your wounds linger and have a hard time healing.
6. You Have Lots of Tummy Troubles

If you have frequent diarrhea, gas or constipation, it could be a sign that your immune system is compromised. Research shows that nearly 70 percent of your immune system is located in your digestive tract. The beneficial bacteria and microorganisms that live there defend your gut from infection and support the immune system. Low amounts of these helpful gut bacteria can leave you at risk to viruses, chronic inflammation and even autoimmune disorders.
7. The other symptoms of a weak immune system can include the following:
Let’s look at the various ways to boost your Immune System in the next blog.
Our immune system is incredibly complicated and essential for our survival. Without an immune system, our bodies would be open to attack from bacteria, viruses, parasites, and more. It is our immune system that keeps us healthy as we drift through a sea of pathogens.
Our immune system is our body’s version of the military - sworn to defend against all who threaten it, both foreign and domestic. Everyone’s immune system is different but, generally, it becomes stronger during adulthood as, by this time, we have been exposed to more pathogens and developed more immunity.
Our immune system protects against disease, infection, and helps us recover after an injury. Several different systems and cell types work in perfect synchrony (most of the time) throughout the body to fight off pathogens and clear up dead cells. It has some interesting soldiers that help make this possible.
Our immune system is a complex fighting system powered by five (5) liters of blood and lymph. Lymph is a clear and colorless liquid that passes throughout the tissues of the body. Together, these two fluids transport all the elements of the immune system so they can do their jobs.
White blood cells charge into battle at any sign of trouble. There are two different types of white blood cells: phagocytes and lymphocytes.

In humans, the blood–brain barrier, blood–cerebrospinal fluid barrier, and similar fluid–brain barriers separate the peripheral immune system from the neuroimmune system, which protects the brain.
These brave soldiers only live up to a few weeks, so it’s a good thing there’s a lot of them — a single drop of blood can contain up to 25,000 white blood cells.

The immune system needs to be able to tell self from non-self. It does this by detecting proteins that are found on the surface of all cells. It learns to ignore its own or self proteins at an early stage.
An antigen is any substance that can spark an immune response. In many cases, an antigen is a bacterium, fungus, virus, toxin, or foreign body. But it can also be one of our own cells that is faulty or dead. Initially, a range of cell types works together to recognize the antigen as an invader.
Your body creates new antibodies whenever it is infected with a new antigen. If the same antigen infects you a second time, your body can quickly make copies of the corresponding antibody to destroy it.
Once an antibody has been produced, a copy remains in the body so that if the same antigen appears again, it can be dealt with more quickly. That is why with some diseases, such as chickenpox, you only get it once as the body has a chickenpox antibody stored, ready and waiting to destroy it next time it arrives. This is called Immunity.
Immunity is the body’s defense system against infection and disease. White blood cells play a key role. Some rush to attack any harmful microbes that invade the body. Other white blood cells become specialists, adapted to fight particular pathogens. All of them work to keep the body as healthy as possible.
There are three types of immunity in humans called innate, adaptive, and passive:
i.) Innate immunity
We are all born with some level of immunity to invaders. Both Human and many animals immune systems, will attack foreign invaders from day one. This innate immunity includes the external barriers of our body — the first line of defence against pathogens — such as the skin and mucous membranes of the throat and gut.
This response provides Fast and General defence. If the pathogen manages to dodge the innate immune system, adaptive or acquired immunity kicks in.

ii.) Adaptive (acquired) immunity
This is a Complex and Targeted Response to Pathogens. This protection to pathogens develops as we go through life. As we are exposed to diseases or get vaccinated, we build up a library of antibodies to different pathogens. This is sometimes referred to as immunological memory because our immune system remembers previous enemies.

iii.) Passive immunity
This type of immunity is “borrowed” from another source, but it does not last indefinitely. For instance, a baby receives antibodies from the mother through the placenta before birth and in breast milk following birth. This passive immunity protects the baby from some infections during the early years of their life.

